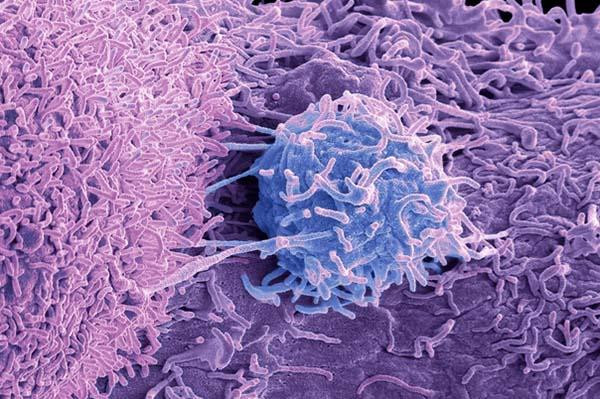
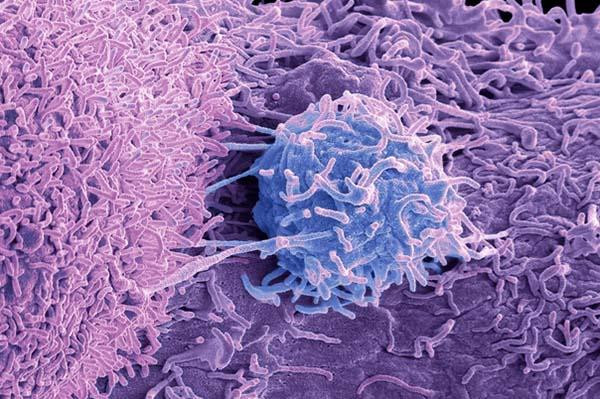
Medications can provide a host of health benefits. They may prevent or eliminate a disease. They might improve your quality of life and even help you live longer. But the medicines we take also have potential side effects. While listed side effects don’t always occur, it’s always possible.
And though that’s unfortunate, it also makes sense: while fighting the good fight against infection, cancer, or other health issues, medicines can also affect normal, healthy parts of the body. That can lead to bothersome symptoms and, sometimes, deadly consequences.
What are the most common and annoying side effects?
If you think you’re experiencing a medication side effect, you can check the National Library of Medicine database for the medicines you take to learn about their side effects.
Among the most common side effects caused by medicines are:
- nausea, constipation, diarrhea
- dry mouth
- drowsiness
- rash
- headache.
While the nature and severity of drug side effects vary widely, some are more bothersome than others. For example, sexual side effects can be especially distressing (and are likely underreported). And forgetfulness or trouble concentrating (often called “brain fog”) can have a serious impact on daily functioning, employment, and quality of life.
Which medication side effects are dangerous?
Though most side effects from medicines are more bothersome than dangerous, there are exceptions. Here are four serious drug side effects that require immediate medical attention.
- Anaphylaxis. This is a sudden allergic reaction affecting many parts of the body, including rash; swelling of the lips, tongue, or throat; and trouble breathing.
- Stevens-Johnson Syndrome (SJS) and toxic epidermal necrolysis (TEN). These two related allergic conditions are marked by severe, widespread rash, skin peeling, and fever. The main difference between them is that skin damage is more severe in TEN. Complications can be life-threatening, such as kidney and lung injury, or skin detachment similar to experiencing a serious burn.
- Drug reaction with eosinophilia and systemic symptoms (DRESS). This rare reaction to medications causes abnormal blood counts, rash, enlarged lymph nodes, and liver injury. Other organs, including the kidneys, lungs, and heart, may be harmed.
What about drug interactions?
Some medicines may cause no side effects until you start taking a second one. That’s because drugs can interact — that is, one drug alters the effects of another drug.
For example, if you take a blood thinner, also taking an anti-inflammatory medicine like ibuprofen or naproxen can suddenly increase your risk of bleeding.
There are thousands of known drug interactions. Medication prescribers, pharmacists, and computerized prescription ordering systems routinely check for them in advance so they can be avoided.
Are medication side effects ever a good thing?
Yes, indeed. In fact, some drugs developed to treat one condition have been approved for something entirely different because of what might be called positive side effects.
That’s how a blood pressure medicine (minoxidil) became a blockbuster treatment for hair loss (Rogaine and other brands). Another medicine (sildenafil), also developed for high blood pressure, was found to trigger erections in men. This lead to its approval as Viagra. There are many other examples of the good side of side effects.
When should you contact your health care provider?
If you suspect you’re experiencing a medication side effect, let your health care provider know. They can help you make the choice that’s best for you.
For serious or dangerous side effects like the examples noted above, it’s important to stop the drug and seek treatment right away. Let the FDA know as well. The FDA welcomes voluntary reporting of serious side effects so they can learn more about a drug’s impact on users, and take steps to improve its safety if necessary. Improvements might include new medication labeling, or even a recall.
For less serious side effects your first inclination might also be to stop the drug. But that’s not always the best choice. While stopping the drug may eliminate the side effect, you’ll also lose the drug’s benefit.
Here are some options your health care provider may suggest:
- Wait. If the side effect is minor, you could decide to put up with it to see if it goes away on its own as your body adjusts to the medication. If time doesn’t help, you may need to decide with your doctor whether the benefits of the medicine outweigh the side effects.
- Reduce. Your health care provider may suggest reducing the dose or how often you take the drug, which may improve or eliminate the side effects.
- Stop. You and your health care provider could decide to stop the medicine and consider a different treatment option, or reconsider whether treatment is still necessary.
- Add. Sometimes it’s reasonable to take a second drug to treat the first drug’s side effects. This option is not ideal. Taking a second drug to treat side effects from the first drug adds yet another medicine to your list. And that second drug could cause its own side effects, or even prompt the need to repeat this sequence with more medications. But sometimes adding another medication is a good option. For example, it’s reasonable to take an over-the-counter medicine (such as acetaminophen or ibuprofen) to treat a mild drug side effect (such as headache). Or if a medicine that causes a significant side effect is actually working well for a serious health condition, then adding a second medicine might make sense.
The bottom line
Drug developers may someday discover the perfect medicine, one that provides major health benefits without any risk of side effects. Until that happens, though, there are many ways to handle drug side effects. The challenge is figuring out which one is best for you.
About the Author
Robert H. Shmerling, MD, Senior Faculty Editor, Harvard Health Publishing; Editorial Advisory Board Member, Harvard Health Publishing
Dr. Robert H. Shmerling is the former clinical chief of the division of rheumatology at Beth Israel Deaconess Medical Center (BIDMC), and is a current member of the corresponding faculty in medicine at Harvard Medical School. … See Full Bio View all posts by Robert H. Shmerling, MD